NEWS BLOG
Medical Administration & IT Careers: Health Informatics Training
Contact: Walter Rodriguez, PhD, PE at wrodrigz@fgcu.edu
Target Audience: Healthcare and administration professionals looking to understand health care information systems.
Tuition: $4000
Financial Assistance: Funding for this program would come directly from participants through tuition. Check if your employer is offering tuition assistance to employees interested in this training.
Duration: 16 Weeks
Online, Self-Paced Modules:
Module 1: Understanding EMR/HER; AHIMA focus geared specifically toward electronic medical records and technology; Health Information Management (HIM) practices being replaced by technology.
Module 2: Understanding the interdependency of Revenue Cycle Informatics on Clinical Informatics and Clinical Care.
Module 3: Differences between Health Informatics requirements for the Hospital, Outpatient, and Ambulatory (Physician Office) settings.
Module 4: Considering deployment methods; HIM/HIS practically applied in the LMHS work environment.
Module 5: Healthcare IT (EHR, single sign-on, meaningful use, PCMH, joint commission, CPOE)
Module 6: Key Topics and Assignments from the textbook below.
Textbook:
Wager, K.A., Health Care Information Systems: A Practical Approach for Health Care Management 3rd Edition. Participants will directly purchase or rent the textbook at http://www.amazon.com/Health-Care-Information-Systems-Management/dp/1118173538/ref=pd_sim_14_6?ie=UTF8&dpID=51AkSEdY4JL&dpSrc=sims&preST=_AC_UL160_SR130%2C160_&refRID=1GYQVR9HSVM33GNAZ9TA
Medical Administration Careers: Medical Scribes Can Learn About Sepsis and SIRS by Watching Videos and Discussing Scenarios
Medical Scribes can learn medical terminology and familiarize themselves with medical procedures by watching videos and discussing scenarios like the one below.
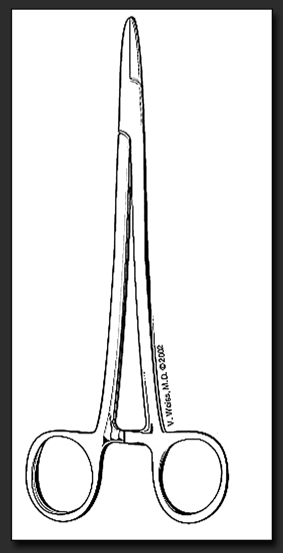
By Walter Rodriguez, PhD and Valerie Weiss, MD
“Sepsis and SIRS are severe conditions that require interventions to counteract. If not treated properly, then multiple organ dysfunction syndrome (MODS) and death may occur.””
Lesson: What is Sepsis? Sepsis is the presence in tissues of harmful bacteria and their toxins, typically through infection of a wound (Ref. https://vimeo.com/129916157). Check also: SIRS
Scenario
Pedro Ramirez is a 67-year old retired veteran who had a routine prostate biopsy in an outpatient hospital facility on Thursday. He was released in the late afternoon and went home with his wife, Gladys. Pedro had a heavy dinner and watched TV with Gladys in their family room. Pedro complained of feeling “crummy” but nothing that a little rest couldn’t fix. Gladys went to bed at 9:30 p.m. leaving him alone. When she awoke at 6:00 a.m. on Friday, and he wasn’t in bed beside her, she went downstairs and found him lying on the family room floor. He was extremely drowsy, shivering, and had urinated on himself.
Gladys called 911. The local EMS arrived and asked his wife what happened. She told them about the prostate biopsy, and that he was fine before she went to bed. She reported that Pedro had taken pre-operative antibiotics, but she didn’t know the name of the antibiotic or dosage. She wasn’t sure which medications he took regularly, as there were many bottles on his dresser.
“Post-operative infection is a broad term which applies to several types of infections a patient can experience as a consequence of undergoing surgery.””
Symptoms of Sepsis
Pedro was drifting in and out of consciousness and was only able to answer the question pertaining to his name. He was taken by ambulance to the local hospital (different than the hospital affiliated with the outpatient facility). The EMS professionals told Gladys to get dressed and meet them at the hospital. Once in the ER, the attending nurse tried to get some pertinent information from Pedro. Unfortunately, all he recalled was his biopsy. Pedro’s vital signs showed:
Temperature of 102.5 degrees F
Blood pressure 88/68 mmHg
Pulse of 122 beats per minute
Respiration rate of 32 breaths per minute
His blood pressure was dropping--he was going into shock.
Coordination of care
Gladys arrived and was told that her husband would be fine; she did not need to worry. However, she was unable to provide any more insight or a list of his meds. She did not know his baseline vital signs. It was Pedro’s first ER experience in this hospital so he had no prior records on file. The ER doctors determined he was in septic shock and once stabilized would be moved to a critical care unit for recovery. Once stabilized, Pedro was able to provide a list of his meds to the nurses. The hospitalist came to see Pedro who said he would contact his primary care physician (PCP) to provide an update. During the next two days (the weekend), numerous tests were administered to Pedro to test for the function of his heart, kidney, liver, etc.
The hospital staff was unable to gain his medical records from the outpatient facility where the prostate biopsy was performed because it was done in another hospital system. On Monday, they were considering a pacemaker because his heart rate was so low. Frustrated by all of the uncertainty, his wife Gladys called the PCP and asked why she wasn’t involved. Dr. de' Medicis, the PCP, said the hospitalist never notified her that her patient of 15 years was in the hospital. She also told Gladys that Pedro had a very low resting heart rate when well and that his current heart rate was normal! At that moment, Dr. de' Medecis (PCP) stepped in and coordinated Pedro’s care with the hospital.
Discussion Questions:
1. How would Electronic Medical Records (EMR) and Electronic Health Records (EHR) help in the above scenario?
2. How would a Medical Scribe assist the Hospitalist and/or the PCP in this scenario?
Healthcare Jobs: Understanding the Difference between Medical Scribes, Medical Transcriptionists, and Medical Billers & Coders
“A medical scribe partners with the physician to perform documentation in the electronic health record.””
By Valerie Weiss, MD
The role of a Medical Scribe
The medical scribe’s primary role is the generation and maintenance of the patient’s medical record, which is created under the supervision of the physician. The medical scribe shadows the physician and documents the patient’s story through the physician’s interaction with the patient. The scribe will also document any procedures performed and the results of any laboratory studies. Scribes document the roadmap of the patient while under the direct care of the physician. A well-written medical record will result in smoother claims processing and provides a medico-legal resource as to the care provided. Because the medical scribe’s role is clinically-focused on observing and documenting the patient’s encounter, many scribes use this invaluable experience as a stepping-stone to further their own education in the health arena.
“Medical scribes become well versed in Medical Terminology as well as Anatomy and Physiology.””
The role of a Medical Transcriptionist
In contrast, a medical transcriptionist, while also in the healthcare field, does not see the patient alongside the physician. Typically, the medical transcriptionist works in a quiet office setting removed from the workflow of seeing patients. The medical transcriptionist’s job is to listen to a physician’s voice dictation and convert that into a written report. A growing trend in medicine is for a physician to utilize voice recognition technology while dictating. The software will convert the physician’s spoken word into a written record. Often, some of the dictation is lost in translation or interpreted incorrectly by the software. A medical transcriptionist’s role, in this case, is to review and edit these medical documents.
The role of a Medical Biller
Even though medical billing and coding are often lumped together, they are actually two distinct jobs. Essentially, a medical biller is a healthcare worker who is tasked with making sure everyone is billed correctly. A medical biller may talk to patients as well as health insurance companies to make sure all invoices are paid correctly and in a timely manner. A medical biller needs to understand coding language and how to read medical invoices.
The role of a Medical Coder
In contrast to a medical biller, a medical coder, does not have communication with the patient or insurance company. The medical coder spends time assessing the medical chart to make sure it is coded with the correct medical codes. Coders must be accurate. Medical coders employ the International Classification of Diseases or ICD. The World Health Organization periodically upgrades the ICD. The current model being used is ICD-10.
Medical Administration Careers: Medical Scribes Understand the 3 Hidden Benefits of Electronic Medical Records for Enhancing the Healthcare of Patients
“Research suggests the importance of accurate and timely patient information to ensure proper care from a quality and safety perspective.” (Broekhuis & van Donk 2011) ”
By W. Rodriguez, PhD [Extracted from: Carstens, D.S., Rodriguez, W. and Wood, M.B. (2014) ‘Task and error analysis balancing benefits over business of electronic medical records’, Int. J. Electronic Healthcare, Vol. 7, No. 4, pp.331–348. The paper was co-authored with Drs. Carstens (FIT) and Wood (Mayo Clinic).]
Background: Amazingly, healthcare spending represents 18% of the U.S. gross domestic product (GDP), and is projected to be 20% by 2020 (Seiden 2012)! And while Information technology (IT) is widely used in everyday life, it is estimated that only 8% of the 5000 hospitals and 17% of the 800,000 physicians in the U.S. use an EMR (Electronic Medical Record) system (Goldman, 2009). Based on a national survey of physicians in 2008, only 4% had a fully functioning EMR and only 13% had a basic system (Mallon, 2009). It is curious that healthcare information technology systems haven’t seen enthusiastic and widespread adoption in an industry, that is, as information and data intensive as healthcare.
Reason: Physicians and hospital administrators simple do not have the time to analyze and implement EMRs in practice. Further, healthcare systems may appear complex and not easily understood at first glance (Mehrjerdi 2013).
Fortunately, Medical Scribes can serve as the link between physicians and this seemingly complex EMR software technology. Medical Scribes can help physicians during the EMR implementation (transition) and beyond.
A study performed by Chircu, Gogan, Boss and Baxter (2013) suggest that during transition times, 40 percent of medication errors, 20 percent of which cause harm, occur from staff miscommunication. Well-trained Medical Scribes can assist physicians reduced medical errors by communicating effectively and recording the physician directions and allowing them to focus on the patient rather than on the technology.
Decrease medical errors: Despite the above challenges, research suggests the importance of accurate and timely patient information to ensure proper care from a quality and safety perspective (Broekhuis & van Donk 2011). Studies provide data that Computerized Physician Order Entry (CPOE) which is another aspect of EMRs enhances patient safety by decreasing medical errors (Krohn 2003). CPOE eliminates illegible orders and most notably the names of drugs, dosages, dosing units, and administration frequency and routes. When associated with decision support function (DSS), alerts for allergies, drug interactions or inappropriate dosing occur in real-time. CPOE with DSS can provide alerts for duplicate tests or inappropriate tests based on a patient’s diagnosis or portfolio of existing test results. Brigham and Women’s Hospital in Boston implementation of a CPOE led to an 81% decline in medical errors, mainly related to decreasing adverse drug events and duplication (Krohn 2003). New York’s Montefiore Medical Center had a 50% decrease in prescribing errors and a 60% improvement in delays between prescription writing and medication administration. Clinical Documentation is another key module of an EMR as it can be designed to permit access to authorized providers involved in the patient’s care useful as a tool for integrating care between multiple different physicians, nurses, therapists and others to include record sharing.
Reduce Cost and Duplication: Cost barriers remain a hurdle associated with EMRs although HIS (Health Information Systems) will decrease global healthcare costs through minimizing duplication, enhancing appropriate test and therapy selection, improving care continuity, integration of services and decreasing avoidable medical errors and accidents (Schmitt et al. 2002; Poon et al. 2004). The difficulty is that patients and payers receive benefits yet the providers of care (doctors and hospitals) are responsible for costs making the “business case” for HIS challenging. Established ROI methodology specifically for IT has been difficult to apply to HIT because of difficulty labeling the benefits with financial metrics but reports suggest EMR improves revenues and reduces costs (Cresswell 2004; Menachemi et al. 2006; Mildon et al. 2001). David Brailer, former National Coordinator for HIT in the Bush administration suggested that a computerized health record system could save $200-300 Billion/year across the U.S. healthcare sector (Goldman, 2009). Hillestad, et al. (2005) by extrapolating the impact of IT from other industries estimated potential national savings of $81 Billion/year by full implementation of an HIT.
Wang, et al. (2003) studied a primary care physician practice that reported an annual financial benefit over a five year period of $86,500 per physician due to cost savings from decreased drug costs and x-ray utilization. Barlow, et al. (2004) reported over five years a cost savings of $140,000/physician due to decreased costs related to transcription, paper chart management and reimbursement recovery. Schmitt, et al. (2002) estimated that the installation and support costs over seven years were $19 Million without quantifying the temporary decrease in physician productivity. By year three, the financial saving exceeded the cost to date, and by year seven, there was an annual savings of $7.5 Million/year related to decreased time processing orders, decreased drug costs and costs due to adverse drug events, transcription costs, chart management costs and increased charge recapture.
California Health care Foundation studied the economic benefit of a fully deployed EMR, and reported a payback period of 2.5 years and thereafter an average gain of $23,000/year/physician despite a decline in productivity initially (Goodman, 2009). Kaushal, et al. (2006) suggested in a hospital setting that ten years of spending $11.8 Million resulted in a savings of $28.5 Million for a net 10 year benefit of $16.7 Million due to drug cost savings, nursing time and the avoidance of adverse drug events. Poon, et al. (2004) reported a net operating benefit by seven years following implementation. Kuperman and Gibson (2002) reviewed reports on the value of CPOE and concluded that it reduces costs but ROI analysis is challenging because baseline costs of key processes are difficult to calculate and several benefits cannot be measured financially. Frisse (2006) suggests that financial ROI analysis of CPOE is inappropriate because “the ROI is measured in safer and more effective medical care.”
Improve Quality of Care: Carroll (2004) suggests that the EMR financial return to a doctor’s practice is lacking. Hamilton (2008) suggests that although EMRs save money it doesn’t go to those that pay for it. Clear recognition of the disconnect between those incurring the cost and those reaping the benefits will be a major step for the widespread adoption of HIT in this country. Moreover, presidential leaders promote a “carrot and stick” approach to finance HIT. The “carrot” is the “HIT for Economic and Clinical Health (HITECH) Act” described by Centers for Medicare & Medicaid Services (2013) and the Congressional Budget Office (2013) which provides a $44,000/physician over a 5 year period for Medicare as an incentive for practices to implement and meet meaningful use standards. The “stick” is that physicians who don’t transition to using an EMR system will see Medicare payments reduced after 2015. Taner, Sezen & Atwat (2012) conducted research where the hospital organization successfully from a financial standpoint implemented technology due to optimizing efficiency through process and workflow improvements. Therefore, process improvement research may help an organization realize savings despite the expenses related to technology such as the EMR as it is essential to understand the operational impact electronic records as hospitals invest in information technology to lower costs and to improve quality of care (Mitchell, S. & Yaylacicegi, U. 2012).
Conclusion: Although EMR implementation is challenging, Medical Scribes can be instrumental in supporting physicians during the transition and beyond.
Medical Administration Careers: 15 Reasons Why Medical Scribes are Valued and Appreciated by Doctors
By Walter Rodriguez, PhD and Valerie Weiss, MD
More and more often, medical scribes are being recognized by physicians in all healthcare settings. Physicians are becoming more aware of the Medical Scribes' qualifications and how they can assist them in their medical practice.
Medical scribes allow for a dynamic conduit between a tangible record and a patient encounter, including the care provided. The role of the medical scribe is more than relevant because physicians are traditionally trained for direct patient care rather than for clerical work.
Below are fifteen (15) reasons why Medical Scribes are valued and appreciated by primary-care clinics, hospitals, healthcare administrators, physicians and specialists.
1. Medical scribes are able to navigate electronic medical records (EMR) with ease, while shadowing a physician. In this way, the physician can focus on the patient, rather than on a computer screen.
The scribe is able to record the physician’s interaction with the patient, including all of the following: physical exam findings, medical decision-making, laboratory results, radiological reports, clinical re-evaluations, consultations, and dispositions. Medical scribes are given unique logins and passwords.
2. Scribes are intimately familiar with HIPAA regulations. In this way, they can maintain the patient's privacy and the institution's security. The federal Health Insurance Portability and Accountability Act was passed in 1996 with a primary goal is "to make it easier for people to keep health insurance, protect the confidentiality and security of healthcare information and help the healthcare industry control administrative costs."
3. Scribes understand the flow of information and the function of the various medical departments in a variety of healthcare settings. i.e., hospitals -- including ED (emergency department) or ER (emergency room).
Scribes are being employed in many arenas of the healthcare field including primary care clinics, hospitals -- including the ED (emergency department) or ER (emergency room), and urgent care centers.
4. Medical scribes understand basic medical terminology and can converse with other members of the medical staff--including hospital administrators, physicians, pharmacists, nurses, medical coders, and so on. If they work with a specialist, they quickly learn highly specialized terms.
5. Scribes become versed in general anatomy and physiology. In their formal certification training, medical scribes are introduced to all of the major organ systems of the body. They understand the "roadmap to the body" and how the organs function. This knowledge provides them with an appreciation of the human body and its complexity.
Many scribes use this knowledge and invaluable experience as a stepping-stone to further education and training in any health-related field.
For example, some medical scribes go on to study nursing or medicine. And some leverage their medical scribe's experience (shadowing the physician) in their application to medical school.
6. Medical Scribes fully understand the methodology of writing of the HPI (History of Present Illness). For instance, scribes are able to record a chronological description of the development of the patient's illness from the first sign and/or symptom or from the previous encounter to the present--including the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms.
7. Scribes are aware of billing codes and principles as they pertain to the medical chart.
A well-written medical record will result in smoother claims processing and provides a medico-legal resource as to the care provided.
8. Medical Scribes are familiar with common medications and will become familiar with specialist's medications, as they go on rounds with physicians.
9. Scribes understand information systems technology, including flow and control of information as well as the technological platforms available.
“they allow for physician to leverage time and see more patients or spend more time with individual patient as less time is spent doing clerical work ... the record may actually be more complete with scribe completing and adding more text or completing ‘meaningful use’ boxes required by third part payers and therefore coding may be more consistent with submitted bill therefore shorter time for reimbursement by the insurance company because chart meets criteria for submitted bill ... lastly, data is better able to be mined and queries submitted which allows for greater chance of meeting quality metrics”
”
10. Medical scribes communicate effectively and are able to use correct medical terminologies. They efficiently take medical notes and accurately record doctor’s patient interaction using electronic tools available.
11. Medical Scribes know the medical scribe tools and information systems available for improving efficiency and effectiveness and healthcare decision-making. They are able to recognize characteristics of various medical scribe systems. In addition, scribes can recognize benefits from various medical scribe systems and understand the cost and issues of various medical scribe systems.
12. Medical Scribes recognize the sources of system threats and ethical implications associated with patient information security and privacy issues, and explain how organizations can address these issues.
13. Scribes recognize network and mobile technologies used in medical practice as well as the issues associated with network and mobile technologies.
14. Medical Scribes can also describe the sources of information security and protection in medical information systems.
Medical scribes recognize the importance of an electronic health record that is connected to the Internet. Thus, they understand the vulnerability of the patient’s chart and the importance of preventing a breach in security.
15. Finally, scribes recognize or describe approaches and technologies that could be used by hospitals to meet the information privacy regulations and standards (technologies and employee training, etc.). They recognize information privacy regulations and standards with which health care facilities must comply. And, more importantly, they recognize the ethical implications of medical scribe information systems.
Medical Administration Careers: 3 Tricks Medical Scribes May Use to Confront Daily Challenges
by Walter Rodriguez, PhD
Eleanor Roosevelt famous quote, “Do one thing every day that scares you,” challenges us to do things that may be uncomfortable at first.
I recalled Eleanor’s advice the first time I found myself looking for a job, after being laid-off from a part-time weekend job … where I traveled throughout Florida helping stage healthcare training seminars. Although the job was very demanding, I thought “I really need to work those extra hours” in order to make ends meet and support my young family.
At the time, I was just in my early 30s, a graduate student at University of Florida, and the father of a 6-year old daughter and a 1-year old son.
By heeding Eleanor’s advice, I was able to confront my fears … rather than despair, I viewed my situation as another challenge. I also made a mental inventory of my skills. For instance, I still had my experience conducting seminars and I was a fairly good learner and teacher.
Well … that’s the short story about how I confronted my challenge, after being fired. The happy ending is that I later graduated from UF and found a great job as an assistant professor. And I am still enjoying what I have done for over 30 years: teaching and trying to help others in similar situations.
Below are three tricks you may use to confront a daily challenge:
1. Visualize yourself being on your desired situation
By using your imagination, you can prepare yourself for success. For instance, if you are looking for a job, you may close your eyes and visualize yourself being on an interview and answering questions with confidence. You imagine talking about your life and work experiences and showing that you enjoy learning new things. Imagine yourself being confident and friendly and visualize your interviewer shaking his/her head in agreement.
2. Find a mentor or adviser or coach
Accept yourself: both your strengths and weaknesses. We all have them. And think “I don’t have to solve all the problems by myself.” You can usually find an experienced friend, family member, mentor or adviser to guide you and help you navigate the rough times. You will be surprised how many people want to help you and your family. Finally, look for challenges and opportunities in your field*.
3. Consistency of Purpose
Once you decide what you want to do, keep doing it every single day, consistently. For instance, if you are looking for a job, keep refining and posting your resume every day. Consider volunteering to work in the community and seeking contacts that will help you with your job search. Of course, if you find yourself lacking the right skill-set and academic preparation, you should consider matriculating in a community college, vocational school or online training program in a high-demand area that you would enjoy.
*What are the Medical Scribe Challenges and Opportunities?
Source: Extracted from a Medical Scribe course developed by Valerie Weiss, MD
"Challenge of Regulatory Requirements: In the medical practice, there are a burdensome amount of documentation requirements (i.e., data, information) that must be entered into a myriad of computer information systems. These system involve a series of complex processes that are employed in hospitals nationwide.
Challenge of Continuous Change: Within each hospital, there are additional frequent changes to what needs to get documented and how. There is so much constant change and mounting documentation responsibility levied on the medical provider that the traditional paradigm of the medical provider who performs his or her own unassisted documentation or dictates into a recorder has proven to be uneconomical, inefficient and unsustainable. To thousands of health professionals who have been chiding at the forced changes to their medical record documentation practices, the silver lining in acclimating to this struggle is scribes.
Job Opportunities: The medical scribe industry has exploded in growth, thanks to the regulatory requirements and changes affecting medical records. For instance, in 2008 there was only 1 medical scribe vendor at the American College of Emergency Physician’s annual conference and approximately 500 scribes nationally. This year, there are 8 vendors and approximately 6,000 scribes. With tremendous growth, comes a natural need to regulate performance. Today, we have the opportunity to do so. If we are to remain in control of our destiny as an industry, we have to establish minimal performance requirements and advocate for compliant practice of appropriate scribe use among medical providers, individual scribes and scribe vendors. If we do not act responsibly with this opportunity then the medical scribe industry will be contaminated by the unscrupulous practice of those who wish to call themselves scribes while engaging in unsupported behavior. By obtaining your scribe certification through the Medical Scribe Certification & Aptitude Test you are distinguishing your training and practice, ensuring that employment as a scribe continues for you and is available for future generations aspiring for a career in the health-related sciences. Certification matters.
Work Environment: The scribe-provider work relationship is a familiar experience to medical providers who were initiated as medical students who learned to work with interns, who likewise learned to work with residents, who likewise learned to work with attending physicians. There are 2 major differences however. Scribes are strictly non-clinical, documentation assistants, and the medical provider is not responsible for teaching the scribe medicine. Notwithstanding the differences, scribes learn a great deal of clinical medicine simply by witnessing and documenting the provider’s interaction with patients. For these reasons, being a scribe is the best job any pre-health major could have."
Medical Administration Careers: Herbal Remedies Making a Comeback and 12 Related Definitions for Medical Scribes
By Peter Reuter, MD, PHD
For most of human history herbal medicines were the number one remedy used by people worldwide. All that gradually changed with the advent of chemistry and pharmacology. Instead of using herbal teas or pastes people started to use standardized drugs produced by pharmaceutical companies, prescribed by medical professionals, and dispensed by pharmacies. Many of these drugs were naturally occurring substances or derivates that had been used as part of herbal medicines for a long time. Aspirin or acetylsalicylic acid (ASA), for example, is a derivative of salicylate, which can be found in such plants as willow tree and myrtle. It was first mentioned as a remedy for pain, fever, and inflammation in an Egyptian papyrus more than 3500 years ago.
Scientists, especially ethnobotanists, went all over the planet in search of other substances from plants, fungi, and lichen that could be tested for their medicinal properties. Over time, however, chemists took over, and more and more pharmaceuticals were created in the lab. That made the process more controlled and made it easier for companies to claim patents on newly synthesized drugs. Yet, approximately 95% of tested components fail in clinical trials and for those few that pass the whole process from start to finish takes about 12 years and costs up to $800 million or more.
That kind of investment is significant for developed countries, but almost too much money for most developing countries, which explains why there are no new drugs coming out of developing countries. It also explains why there are only few and often no recently introduced drugs for rare disorders or disorders that mainly occur in poorer countries. Malaria is a typical example for that. Although there are an estimated 200 million cases of malaria every year and about half a million deaths related to malaria, there hasn’t been a new drug to treat malaria since artemisinin-based combination therapy (ACT) was introduced in the 1990s. One of the reasons for companies not investing into the development of new antimalarial drugs is that about 85% of all cases occur in Africa, where people can only afford to get the drug if governments or international non-governmental organizations (NGOs) subsidize the costs of treatment.
Starting in the mid 1990s, a new approach developed that looked into traditional herbal medicines and their efficacy in treating certain diseases. For example, researchers in India conducted a nationwide survey of Ayurvedic physicians to take inventory of herbs used to treat conditions such as arthritis, diabetes, and hepatitis. After they had identified certain herbs for treatment of arthritis they started observational studies in a clinical setting as well as animal studies. Because this approach reverses the order in which traditional pharmacology works, it is usually called reverse pharmacology.
In the case of malaria, reverse pharmacology pointed to the benefits of Mexican prickly poppy (Argemone Mexicana) for the treatment of milder cases of malaria. Although the poppy was native to Mexico, it somehow made its way to Africa sometime in the 1800s and soon became a part of herbal remedies. When researchers talked to traditional healers in Mali in West Africa they learned about the beneficial effect of Argemone tea on patients with mild malaria. That led to a first prospective study that compared using Argemone tea for half of the patients and a standard artemisinin-based combination therapy (ACT) for the other half. Surprisingly Argemone tea did almost as well as ACT therapy in patients with non-life threatening malaria, although it hadn’t been refined and patients just drank as much tea as they liked.
But, there are still a lot of scientists, especially in pharmacology, that are skeptical or outright opposed to this approach. They prefer to use well-defined compounds and point to the fact that herbal remedies often contain a mix of many active substances that may cancel each other out or cause uncontrollable side effects. Teas and infusions are almost impossible to standardize, which makes it difficult to give exact doses of active ingredients to the patients. They also point to unknown toxicities of plants or parts of plants. When we look at Mexican poppy, for example, then we find that the poppy seeds contain the poison sanguinarine, which was implicated in a mass poisoning of 3000 people in India in 1998 that lead to the death of 65 people. The leaves, however, are nonpoisonous and its tea is safe to consume.
Another success story for reverse pharmacology and herbal remedies is happening in the western Pacific. Palau is an island nation of more than 500 islands that is a paradise for scuba diving and snorkeling. However, Palau also has the seventh highest obesity rate on the planet and many inhabitants suffer from high blood pressure (hypertension) and diabetes. Instead of relying on the tried-and-true methods that failed to stop the obesity epidemic in western developed countries, doctors tried to find herbal remedies to help treat hypertension and diabetes. After analyzing traditional herbal medicines, they were able to draw up a list of herbs that showed potential. In the end two plants, Morinda citrifolica (a tree from the coffee family), and Phaleria nisidai, were associated with weight loss (M. citrifolica) and lowering of high blood pressure (P. nisidai).
Finding scientific proof that traditional herbal remedies are almost as good for the treatment of a variety of diseases as modern drugs while often having far fewer side effects is a boost to many who look for a more holistic approach to medicine. Many people in developed and developing countries are trying to live a more healthy life by eating local and often organic produce, by cutting down on animal protein, and by using traditional remedies when possible and available. The more their number grows, the more companies will try to cater to their needs and demands, and the more herbal remedies will be used to treat physical and mental health disorders.
© Peter Reuter 2015
Malaria video: https://www.youtube.com/watch?v=jayoAFAtGQY
Ayurvedic medicine video: https://www.youtube.com/watch?v=sDtIs8p0Uuc
Herbal Remedies Making a Comeback - Definitions
Pharmacology: The study of chemical and biological substances, their effects on living systems and their use to influence biological systems.
Derivative: In chemistry a substance that is based on or derived from another substance.
Aspirin: Also known as acetylsalicylic acid. A pain killer (analgesic) based on salicylic acid, which is found in the bark of willow trees. The bark has been used for at least 2500 years to treat pain, fever, and inflammation. The chemical compound was first created by German chemists in the mid-1800s and sold under the name aspirin by the pharmaceutical company Bayer starting in 1897. It is nowadays used to treat pain, fever, inflammatory diseases (e.g., rheumatic arthritis), and to prevent heart attacks and some forms of cancer.
Willow tree: Name for a subfamily of deciduous trees and shrub found in cold and temperate regions on the northern hemisphere. The bark of willow trees has been used for at least 2500 years to treat pain, fever, and inflammation
Artemisinin: A drug against malaria isolated from sweet wormwood (Artemisia annua). Artemisinin and its related substances are the most commonly used drug against uncomplicated cases of malaria caused by Plasmodium falciparum.
Arthritis: Inflammation of one or more joints leading to pain, swelling and stiffness. Acute forms of arthritis are usually caused by bacteria. Common chronic forms are osteoarthritis (wear-and-tear arthritis often caused by overloading the joint and overweight) and rheumatoid arthritis (an autoimmune disease in which the body attacks its own joints). The treatment depends on the underlying cause of the inflammation.
Diabetes: Also known as diabetes mellitus. Generic term for a group of diseases with abnormally high levels of glucose in the blood. In type 1 diabetes (10% of cases) the body doesn’t produce any insulin (the hormone that helps glucose enter the cells where it will be burnt to release its energy), whereas in type 2 (90% of cases) the cells don’t respond to insulin properly. High blood sugar levels cause a variety of complications such as glaucoma, cataract, skin ulcers, heart disease, high blood pressure, stroke and kidney failure to name just a few.
Hepatitis: Inflammation of the liver caused by a variety in causes, most commonly viruses (hepatitis A, B, C), chronic excessive alcohol intake, and prescription and recreational drugs. Acute hepatitis can be fatal, heal on its own or take a chronic turn. Chronic hepatitis is often subclinical in presentation with few or no symptoms at all, but more often than not leads to scar formation (fibrosis) or chronic liver failure (cirrhosis) that cannot be cured unless the patients receive a liver transplant. Chronic hepatitis also increases the risk for developing liver cancer.
Obesity: The Body Mass Index (BMI) is used to classify people based on body weight and height into underweight, (BMI below 20) normal body weight (BMI between 20 and 25), overweight (BMI between 25 and 30) and obese (BMI above 30). Even though those ranges aren’t a law of nature and may be changed depending on future research, we still know that the heavier people get the more likely they are to develop diseases of the cardiovascular system, diabetes mellitus type II, and osteoarthritis. Currently approximately 1/3 of Americans are of normal weight, 1/3 is overweight, and 1/3 is considered obese.
Hypertension: Also known as high blood pressure. A blood pressure of 140/90 or above at rest is considered as hypertension. There are some known risk factors that increase people’s chances of getting high blood pressure, such as obesity, too much salt in the body, smoking, and lack of exercise. However, 85% of all people with high blood pressure have no known risk factor or underlying cause and the disease cannot be cured only modified. High blood pressure doesn’t cause symptoms for most patients for many years, which explains why it goes often undiagnosed for a long time. Untreated high blood pressure can lead to heart attack, stroke, blindness, and kidney failure
Holistic medicine: A system of alternative healthcare that considers the whole person, body, mind, and spirit, instead of focusing on physical symptoms only. There is, however, no consensus what holistic medicine actually is and does. For some practitioners it is the combination of mainstream medicine with traditional medicine and herbal remedies, for others the focus is more on working with the mind, spirit and emotions of the patients.
Medical Administration Careers: 3 Ways for Learning Medical Scribe Terminology and New Healthcare Definitions
by Walter Rodriguez, PhD
Passing medical certification exams and tests are one of the most challenging tasks you may encounter---even with seemingly adequate preparation! And, after passing the certification exams or tests, you must still keep current with the new medical terms and healthcare definitions. So, what can you do to stay current with the medical terminology and healthcare definitions?
Below are three authoritative (research-tested) ways you may use to learn current and new medical terminology:
1. Read Medical News and Blogs: One of the best ways to learn medical terminology is by reading articles in refereed journals and institutional blogs like this one. Reading the terms in the context of an article will help you retain the knowledge. After reading this blog, please scroll down to read sample articles written by Dr. Peter Reuter, an assistant professor in the College of Health Professions and Social Work at Florida Gulf Coast University and author of multiple medical encyclopedias & a web resource.
2. Review Electronic Flashcards: In preparation for a test, we tell our students to go to interactive resources, such as Quizlet. Please see an example at https://quizlet.com/11256201/basic-medical-terminology-scribe-flash-cards/. In addition, we provide numerous practice quizzes on our Canvas Learning Management System (LMS).
3. Take a Diagnostic Exam: According to How We Learn: The Surprising Truth About When, Where, and Why It Happens by Benedict Carey, "taking a test before you know anything about it improves subsequent learning." In our Medical Scribe Program and courses, we have developed worry-free diagnostic tests that students take before they start learning some of the medical scribe and medical terminology materials. These types of exams help us (faculty) diagnose (identify and analyze) where we need to focus our teaching and learning efforts. And when we start our Medical Scribe courses and programs, we always provide at least one diagnostic test. The tests help us benchmark the students' learning progress.
Please visit again for additional hints on how to learn Medical Terminology to pass your Medical Scribe certification exams, even without registering for one of our online courses. For more information or to try one of the exams, please complete this form.
Medical Administration Careers: Postoperative Delirium - A Potentially Serious Issue for Older Patients. [And a few terms* that Medical Scribes should be familiar with.]
Peter Reuter, MD, PhD
General anesthesia has been around since the mid-1800s, and every year millions of people undergo procedures that require general anesthesia. What may be surprising to most people is the fact that after using anesthetic drugs for approximately 170 years, we still don’t know how they act exactly. We can explain how they block or suppress pain signals, but we still don’t have a sufficient explanation as to how they induce unconsciousness that can be reversed. We have evidence that they act on nerve cells or neurons in a way that interferes with the regulation of sleep, attention, and memory, and there is speculation that they disrupt communication between different parts of the brain, which somehow causes unconsciousness.
Initially patients undergoing general anesthesia were mostly younger patients because of the risks associated with the procedure, especially the stress put on the cardiovascular and respiratory systems. However, over time anesthesia has become safer for all patients and surgeons started to perform elective procedures on patients that would have been excluded because of their advanced age in the first part of the last century. Combined with an increasing number of people living into their 70s, 80s, and 90s the number of older people undergoing general anesthesia has skyrocket in the last 50 years.
In the early 1980s reports surfaced that described patients going through a state of confusion, hallucinations and memory loss after general anesthesia. The patients couldn’t respond to normal questions, such as how they were feeling, and often replied with nonsensical answers. Over time this state was termed Postoperative Delirium. When doctors started to look into the cause for this state they couldn’t find a relationship to the kind of anesthetic used or the duration of the anesthesia. There were, however, first indications that the delirium wasn’t always just a transitional state that lasts a few hours only, but could linger for months and, in rare cases, even for years.
What makes it difficult to identify the underlying cause, if the anesthetic isn’t to blame, is the fact that the stress of the general anesthesia is just one of many stresses the patients are under during their time in the hospital. Just being hospitalized for an acute or chronic ailment and the changes that come with that, such as loss of privacy, inability to sleep properly, changes to the diet or having to change or take new medications, can sometimes cause patients to become confused, depressed, irritable or even delusional. Two factors that have been isolated by various researchers are age and the type of surgery performed. We now know that patients above 70 years of age are more prone to develop Postoperative Delirium. The risk increases even more if they already suffer from mental deficits, such as dementia, before the anesthesia. Even patients who had just mild symptoms, such as forgetting appointments or to take their medication on time, were shown to be more likely to go through the delirium. Major surgeries that sometimes last for hours and that require the patients to stay in the hospital overnight or longer, also carry an increased risk for developing the syndrome. Studies have shown that half of patients older than 60 go through a state of confusion and disorientation after heart bypass or heart valve replacement surgery. Hip replacement surgery, which is usually faster and an elective procedure that can be done when the patient is physically and mentally ready, has a far lower incidence for the same age group.
Studies have also shown that some type of regional anesthesia can increase the risk for Postoperative Delirium as well. Normally, regional anesthesia uses an anesthetic drug to block nerve signals from a certain area of the body, such as the legs, from reaching the spinal cord. The patient loses feeling in the area, but is of course alert. However, patients are often given a sedative drug, such as propofol, to calm them down and reduce the stress of the situation. If the amount of those sedative drugs is sufficiently high patients go through a state of general anesthesia during at least some part of the procedure without them, and often the anesthetist, being aware of that.
Not only are older patients more susceptible to developing Postoperative Delirium, it often lasts longer and is more severe. Having older patients show signs of a mental slowdown (performing poorly on word recall test for example) three months after major surgery is not uncommon, with the time until complete recovery easily stretching to six to twelve months. One of the reasons could be that the nerve cells in older patients get more easily overwhelmed by anesthetic drugs and take a much longer time to recover their preoperative function. There is also speculation that some of the connections between different parts of the brain that get disrupted by general anesthetics, may take longer to be restored in older brains or may not be restored completely leading to lingering aftereffects.
One way to lower the risk for Postoperative Delirium is to make sure the patients are well nourished and especially well hydrated before surgery. Chronic dehydration, due to an aging thirst center that doesn’t alert the older patients any more of a lack of water, is a common problem among older people and can on its own lead to mental confusion. A more surprising find was that family and friends can play an important role in preventing and minimizing Postoperative Delirium. Patients that are accompanied by relatives or friends or who receive visits from them postoperatively have lower rates of confusion and better outcomes overall than patients that are unaccompanied and don’t have visitors. How these social interactions help prevent and treat Postoperative Delirium is unclear, however, the benefits are so tangible that more and more hospitals encourage relatives to stay with older patients before and after general anesthesia.
* Note for Medical Scribe students: Please see definitions below.
© Peter Reuter 2015
Video links:
General anesthesia: https://www.youtube.com/watch?v=vRlk73BbQ8o
Delirium: https://www.youtube.com/watch?v=hwz9M2jZi_o
Definitions
Anesthesia: The word itself means lack of feeling or freedom from pain, but is generally used to describe a method that reduces pain and feeling in a certain area (local anesthesia), region of the body (regional anesthesia) or the body as whole (general anesthesia). It is based on the application of substances (anesthetics) that interfere with the transmission of signals in nerves to the central nervous system (brain and spinal cord). Because of the lack of sensation and numbing of pain doctors can operate on patients using one of those techniques.
Unconsciousness: A state during with a person is not consciously aware of stimuli from the environment or its own body and is unable to respond. It can be a reversible state, such as coma or general anesthesia, or a permanent stage with no recovery.
Cardiovascular System: Consists of the heart (cardio-) and blood vessels (vascular). Its task is to supply sufficient amounts of blood to any part of the body at any time and under any conditions. To do that it has to pump a sufficient amount of blood, which can be 4-5 times more under physical stress than at rest, while generating an adequate blood pressure to push the blood through 50,000 miles or more of blood vessels.
Respiratory system: Consists of upper and lower airways that transport air into and out of the lungs and the lungs where the exchange of oxygen (into the blood) and carbon dioxide (out of the blood) happens. The task of the respiratory system is to supply sufficient amounts of oxygen regardless of how much the body needs and to remove poisonous carbon dioxide from the blood.
Delirium: Also known as acute confusional state. A serious, but usually temporary and reversible, state of impaired brain function with confusion and sometimes hallucinations and hyperactivity. Can be seen I high fever, intoxication (chronic alcoholism often leads to delirium tremens), and other disorders.
Dementia: General term to describe a decline in mental abilities that is severe enough to effect daily life. Dementia is not a disease itself, but a symptom of other diseases and can also be considered part of a normal decline in higher age, which it is also often called senility. The most well known type of dementia is dementia caused by Alzheimer’s disease.
Heart bypass: Surgical procedure to bypass a blocked blood vessel (coronary artery) be connecting the area before the blockage and the area behind the blockage by inserting a healthy blood vessel (graft) from another area of the same patient. Originally the surgery required to stop the heart from beating during the procedure and surgeons had to use external pumps to keep blood flowing through the body. Nowadays the procedure is done on the beating heart.
Heart valve replacement: Heart valves regulate the flow of blood thought he heart, just like valves regulate the inflow and outflow of air and gasoline in car engines. Defective heart valve that either don’t open properly (stenosis) or fail to close completely (regurgitation) effect the flow of blood and put extra stress on the heart, which can lead to heart attacks and death in the long term. Heart valves can be replaced using mechanical valves, animal valves (pigs) or donated human valves.
Propofol: A short-acting anesthetic used to induce or maintain anesthesia. It became infamous when it was discovered that the late Michael Jackson had received propofol iv injections to combat his insomnia, which may have caused or contributed to his death.
Medical Administration Careers: Bacteria Are Your Best Friend. And a few definitions medical scribes and healthcare students should be aware of.
Peter Reuter, MD, PhD
It has been known for a long time that there are many bacteria that grow on the body membranes that cover our outer (skin) and inner body surfaces (mouth, gastrointestinal tract, vagina). Many of them will cause disease when they overgrow an area, while others will never harm us or can even help protect us from disease causing microbes (so-called pathogens). We knew that some pathogens could cause severe diseases when introduced into our gastrointestinal system, such as food poisoning. It has also been known for quite some time that some of these bacteria help us break down certain food we eat, which can be beneficial, but can also cause irritation and embarrassment (beans, beans the magic fruit…). However, there were also indications that at least some bacteria have an even greater and more beneficial influence on what is going on inside our body, such as strengthening our immune system.
Over the last 10 years or so our understanding of and appreciation for the bacterial garden, especially inside our mouth and the large intestine has grown tremendously. We now estimate that for each cell in our whole body we have 10 bacteria colonizing our large intestine. Researchers have found that there are many different bacteria that together form a so-called microbiome. Which bacteria are dominant in a person’s microbiome is of great importance for how their body processes food, how many calories we extract from the food we eat and how our body weight develops.
Over the last few decades almost all developed countries have experienced an ever-increasing weight problem. Although no one really knows what a “normal” weight is, long-term research has shown that overweight people are at a higher risk to develop certain diseases. The Body Mass Index (BMI) or Quetelet index is used to classify people based on body weight and height into normal body weight (BMI below 25), overweight (BMI between 25 and 30) and obese (BMI above 30). Even though those ranges aren’t a law of nature and may be changed depending on future research, we still know that the heavier people get the more likely they are to develop cardiovascular system diseases, diabetes mellitus type II, and osteoarthritis. Currently approximately 1/3 of Americans are of normal weight, 1/3 are overweight, and 1/3 are considered obese.
Because of the negative long-term effects for overweight and obese people themselves as well as the enormous financial burden treatment of their obesity-related diseases puts on society as a whole, there have been many attempts at educating people about the dangers of obesity and the benefits of weight loss. Still, the percentage of overweight and obese adult and children keeps rising steadily. Researchers looking into these issues kept coming across people who seemed to do everything right, they ate healthy food in recommended amounts and exercised, but couldn’t lose weight or even gained some more, whereas others seemed to do everything wrong, from eating too much unhealthy food to not exercising at all, and yet didn’t gain any weight. We couldn’t find any reason for this difference when we measured how much energy they burnt at rest (basal metabolic rate, BMR) or when active (total metabolic rate, TMR), which indicated that there had to be something to how these different people digested food and absorbed nutrients.
The first hints about the importance of our gut bacteria for our body weight came from twin studies. They showed that “lean” twins and “obese” twins had different bacterial floras. When they ate the same kind and amount of food the lean twins would stay lean, while the obese twins gained more weight. We also saw the importance of a healthy microbiome when we looked at the reasons for severe bacterial infections of the large intestine caused by antibiotics given for the treatment of bacterial infections. One of the most surprising findings, however, was the importance of natural birth and breastfeeding on the long-term body weight of babies and children. Babies born via C section and babies raised on formula instead of breast milk have a much higher chance of becoming overweight or obese. Looking into this topic, we realized that babies pick up a healthy bacterial flora on their way through the birth canal of the mother. These bacteria colonize the skin, the mouth and the large intestine of the newborn and establish a healthy environment. Breastfeeding encourages further growth of this healthy microbiome. Babies delivered via C-section don’t pick up bacteria on their way out of the womb and babies fed on formula grow bacteria that breast-fed babies start growing once they transition to solid food. As their immune system had time to develop first they are more likely to being able to resist and suppress unhealthy microbes.
Based on these findings some researchers in Europe are experimenting with transferring healthy gut bacteria from lean patients to overweight patients to help them lose weight. Most doctors, however, want to wait and find out first which bacteria really are the good guys. In this way, we can isolate them and then introduce them into the body of overweight people. But, there are situations where a transfer of gut flora is a potentially life-saving procedure. Some patients on antibiotics or after gastroenteritis develop a Clostridium difficile infection in their bowels, which can cause vomiting, diarrhea and abdominal pain, and even be fatal in severe cases. One way to treat this disorder is to perform a fecal microbiota transplant – sometimes jokingly referred to as transpoosion. In this procedure a fecal sample of a healthy donor is introduced into the rectum of the patient. In a recently reported case from the United Kingdom a mother suffering from this condition was given a fecal transplant from her overweight daughter. The transplant did its job, the bowel infection healed, but the mother gained 36 lbs of weight over the next sixteen months going from a BMI of 26 (just above normal weight) to a BMI of 34.5, which is classified as obese, under the same diet as before.
There is still a lot to be learned about how bacteria influence our body as a whole and how we can use them to treat and prevent acute and chronic disorders. But, we can already say that bacteria, not dogs, should be considered men’s best friend.
© Peter Reuter 2015
Videos:
Bacteria: https://www.youtube.com/watch?v=qCn92mbWxd4
Body Mass Index: https://www.youtube.com/watch?v=1PyrXtYON1k
Definitions
Microbe: Microorganism that can cause disease or fermentation on carbohydrates
Pathogen: Also known as infectious agent. General term for anything that can cause disease in a human, animal or plant. Most often used for microorganisms, such as bacteria, viruses, fungi, and parasites.
Gastrointestinal system: Also known as digestive system. Organ system consisting of the gastrointestinal tract (mouth, gullet, stomach, small and large intestine) and accessory structures, such as teeth, tongue, salivary glands, liver, gallbladder and pancreas. It has to break down (digest) foodstuff and drinks to prepare nutrients, such as glucose, to be taken into our body.
Large intestine: Also known as large bowel and (mistakenly) colon. The last part of the digestive tract starts with the cecum, a blind-ending sack with a worm-like appendage called appendix vermiformis, and end with the anal canal. The longest part, the colon, starts at the right lower abdomen. It has four parts, ascending, transvers, descending, and sigmoid colon. The rectum, so called because it is straight, connects colon and anal canal. The colon isn’t important for nutrient uptake, apart from water and salt, which is why it is not essential to life and can be removed completely if needed.
Basal metabolic rate: The amount of energy expended by the body while at rest in a neutrally temperate environment. It is higher during childhood and teenage years and keeps declining throughout adulthood. Women have a fairly constant BMR between approx. 25 and 45, which makes it easier for them to keep their weight constant compared to men, who have a higher BMR during teenage years and early adulthood.
Total metabolic rate: The total amount of energy used by our body when we’re active. It depends on our basal metabolic rate (higher for men than women) and the level of physical activity, the more active we are the more energy we use and the more energy (calories) we can consume without gaining weight.
Bacterial flora: All the bacteria living in our digestive system form one big ecosystem. Depending on where we life, what we eat and drink and so on the composition of this flora changes. While most of the bacteria are harmless or beneficial for us, some of them can cause serious illness when they overgrow the others. Intestinal bacteria that find their way into the bladder or other parts of the urinary tract are by far (up to 90%) the most common cause of urinary tract infections (UTI).
Antibiotics: Substances that can fight and sometimes kill microorganisms, especially bacteria, that can cause diseases in human, animal, or plants.
C section: Also known as Caesarean section. A surgical intervention to deliver the baby through the wall of the abdomen and the womb (uterus). The surgeon has to cut through the abdominal wall and the wall of the womb to get access to the unborn baby. The surgeon has to work fast, because of the danger to mother and child, but also be careful not to cause harm to the baby when cutting through the womb.
Gastroenteritis: Originally to describe any inflammation (-it is) of the stomach (gaster) and guts (enteron) the term is now mostly used for any illness of the digestive tract that leads to diarrhea, nausea, vomiting, and/or crampy abdominal pain. Most cases are caused by viruses, such as an outbreak of Norwalk virus on cruise ships, or bacteria (classic food poisoning).
Clostridium difficile: Bacterium that lives in our intestines without causing any issue until it overgrows other bacteria, which is often caused by antibiotics therapy. Infection can cause severe gastroenteritis and death in rare cases. It is related to Clostridium botulinum, which produces a variety of toxins among them botox, which has found a lot of uses in medicine.